Dental surgery
At the Aldent Comprehensive Dentistry Center, we perform a wide range of surgical procedures within the oral cavity. Thanks to modern technologies and the knowledge and experience of our qualified oral surgeons, we guarantee safety and comfort during all procedures.
Comfort and Precision First
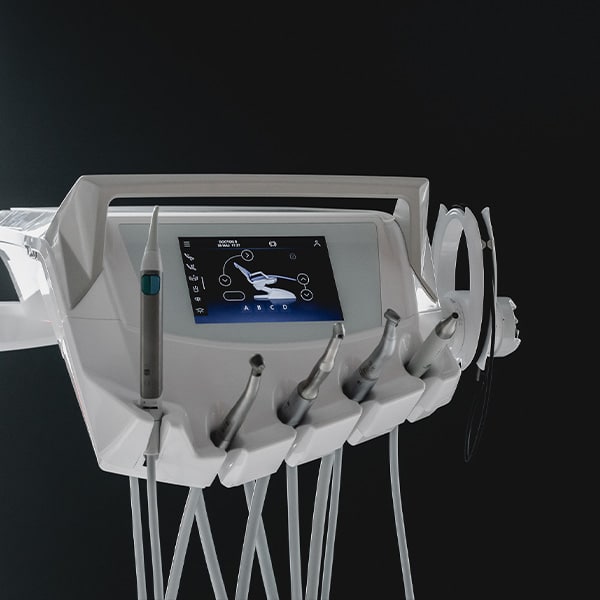
The Most Advanced Computerized Anesthesia
For the full comfort of our patients, all oral surgery procedures are performed using computerized anesthesia systems – Sleeper One and Quick Sleeper.
These devices control the delivery of the anesthetic with microprocessors, which eliminates the pain associated with the pressure of the anesthetic fluid.
The use of these devices minimizes patient stress related to the sight of a traditional syringe.


Electrosurgery – Precision and Effectiveness
At our clinic, we use the TCS II electrosurgical knife, which allows for bloodless surgical procedures. Electrosurgery is a proven therapeutic method that has been used for many years in both dentistry and medicine.
To cut and coagulate soft tissue, electrosurgery utilizes radio frequency energy similar to that used in broadcasting. The concentration of radio frequency energy in a small active electrode enables tissue cutting and coagulation. While the active electrode itself remains cold, sufficient energy is generated along its path to effectively cut and coagulate.
Cutting with a scalpel causes crushing and tearing of the tissue. In contrast, electrosurgical cutting leads to the vaporization and evaporation of tissue along the electrode’s path.
When the output power is properly adjusted, the electrode cuts without resistance, allowing for precision and high control of movement. This method enables effective bleeding control, better access to caries, and gum contouring.
Innovative Surgical Techniques
Sonic Line – Safe and Minimally Invasive Procedures
In our clinics, we use the innovative Sonic Line device from Komet, which, thanks to precise cuts and controlled vibration amplitude, ensures gentleness and safety during procedures.
By using a sonic tip, we achieve: very delicate incisions, excellent visibility and the ability for detailed control, safety (protection of soft tissues), and bone preservation (thanks to high-precision cutting tips, linear vibrations, and controlled, consistent amplitude).
This technology allows for precise incisions while minimizing post-operative pain and simultaneously protecting soft tissues.


Laser Biostimulation Therapy
To accelerate tissue healing, we use laser biostimulation therapy. With a biostimulation laser, we treat mucosal diseases, provide anesthesia, accelerate healing, and stop bleeding.
Thanks to its sterilizing properties, the laser has anti-inflammatory and anti-swelling effects. It has been proven that the biostimulatory properties of the laser increase antibody production, stimulating the immune system and supporting faster wound healing after procedures such as extractions, frenectomy incisions, and resections. It also reduces the risk of infection and accelerates tissue regeneration.
The biostimulation laser supports and improves the quality of treatment in cases of periodontal abscesses, swelling, pulpitis, and chronic periapical tissue inflammation. It is an ideal tool for reducing bleeding and eliminating inflammatory foci.
All these excellent features of the biostimulation laser make visits to our clinics pleasant and comfortable.
Stages of Surgical Treatment
During the first visit to our Center, we conduct a detailed medical interview to better understand the patient’s health history and current concerns. We then examine the oral cavity to assess the need for surgical intervention.
Computerized Local Anesthesia
All surgical procedures in our clinic are performed under computerized local anesthesia. We use advanced devices such as Sleeper One and Quick Sleeper, which control the delivery of the anesthetic, ensuring full comfort and eliminating pain.
Healing Assessment
During the follow-up visit, we check the condition of the soft tissue healing and, if necessary, remove the stitches. We make sure that the healing process proceeds correctly and without complications.
Specialized Surgical Procedures at CSK ALDENT
Removal of Permanent and Primary Teeth
Extractions are necessary in the case of teeth destroyed by decay or remaining tooth fragments. We perform these procedures for both adults and children, ensuring full patient comfort and safety. Extractions are carried out under computerized local or conduction anesthesia, minimizing pain and stress associated with the procedure.
Orthodontic Extractions
Sometimes it is necessary to remove teeth for orthodontic reasons, to allow proper alignment of the remaining teeth within the dental arch. We perform these procedures with the highest precision while providing appropriate post-extraction care.
Socket Preservation with Bone Substitute Material
To maintain bone structure and gum aesthetics for future implant-prosthetic work, we offer extractions combined with socket preservation using bone substitute material. This prevents bone resorption and allows for better preparation for subsequent prosthetic procedures.

Impacted teeth, such as canines and third molars (also known as wisdom teeth), can pose a serious dental problem when they do not erupt properly. Incorrect positioning, rotation, or lack of space in the dental arch may lead to numerous health complications. In such cases, surgical exposure of these teeth through specialized oral surgery is necessary.
Causes and Consequences of Impacted Teeth
Impacted teeth can have various causes, including:
- Genetic predisposition
- Lack of space in the dental arch
- Incorrect eruption angle
- Mechanical obstacles such as other teeth or soft tissues
The consequences of untreated impacted teeth may include:
- Pain and swelling
- Inflammation and infection
- Shifting and deformation of adjacent teeth
- Formation of cysts and tumors

Process of Impacted Tooth Exposure
Consultation and Diagnostics
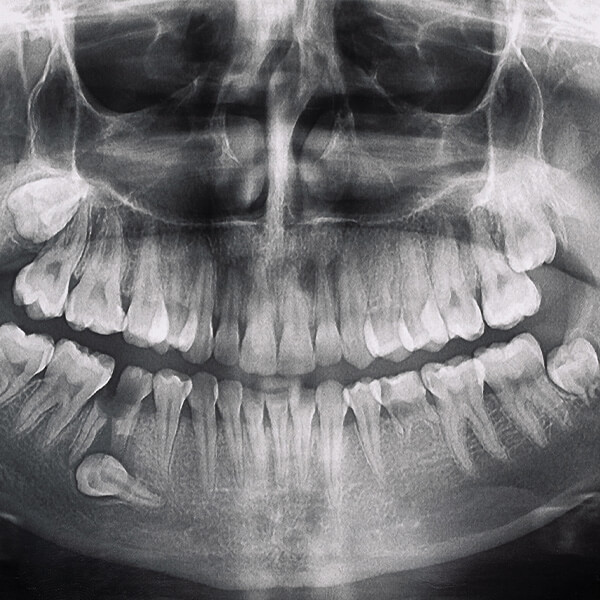
The first step in treating impacted teeth is a detailed dental consultation and diagnostics. We perform panoramic X-rays and cone beam computed tomography (CBCT) to accurately assess the position of the impacted tooth and its effect on surrounding tissues and dental structures.
Treatment Planning
Based on the diagnostic results, we create an individualized treatment plan. We explain the procedure to the patient, discuss possible risks and benefits, and provide detailed information on preparation for surgery and postoperative care.
Surgical Procedure
The exposure of impacted teeth is performed with the highest precision and attention to patient comfort. The procedure is carried out under local anesthesia, minimizing pain and stress.
Stages of the Procedure
- Anesthesia: Local anesthesia is administered so that the patient feels no pain during the procedure.
- Gum incision: The surgeon makes an incision in the gum to access the impacted tooth.
- Removal of obstructions: In some cases, it may be necessary to remove bone fragments or reposition adjacent teeth to fully expose the impacted tooth.
- Exposure and possible extraction of the tooth: Once exposed, the surgeon assesses whether the tooth can be preserved and aided in eruption, or if extraction is necessary.
- Wound closure: At the end of the procedure, the wound is thoroughly cleaned and closed with sutures.
Postoperative Care
After the procedure, the patient receives detailed postoperative care instructions, including ways to minimize swelling, pain, and infection risk. We recommend applying cold compresses, taking prescribed painkillers and anti-inflammatory medications, and avoiding strenuous physical activity for several days after surgery.
Follow-Up and Monitoring
Regular follow-up visits allow us to monitor the healing process and evaluate the results of the procedure. If necessary, we take additional steps to ensure complete and rapid recovery.
Indications for Extraction
The removal of wisdom teeth, also known as third molars, may be necessary for various reasons. Below are the most common indications for this procedure:
Orthodontic Indications
Wisdom teeth often do not have enough space to erupt properly in the dental arch, which can cause the shifting of other teeth. Removing third molars is often recommended as part of orthodontic treatment to prevent crowding and maintain proper occlusion.
Incorrect Tooth Position
Wisdom teeth may erupt at an angle, causing impaction in the jawbone or maxilla. Such positioning can damage neighboring teeth, bone, and soft tissues, as well as lead to cyst formation and infections.
Recurrent Infections
Partially erupted wisdom teeth are especially prone to bacterial infections. Food debris and bacteria can accumulate around them, causing recurring inflammation, swelling, pain, and difficulty opening the mouth.
Pressure on Adjacent Teeth
Erupting wisdom teeth may exert pressure on neighboring teeth, leading to pain and damage. In severe cases, this can also cause resorption of the adjacent tooth roots.
Neuralgia
Improperly erupting wisdom teeth can press on nerves, causing intense neuralgic pain radiating to the jaw, ears, head, and neck. Removing these teeth can bring relief and improve the patient’s quality of life.


Procedure
Preparation
Before the procedure, the patient undergoes a detailed dental consultation, which includes an oral examination and imaging diagnostics (panoramic X-ray, CT scan). Based on this, we create an individualized treatment plan.
Anesthesia
The removal of wisdom teeth is performed under computerized local anesthesia, ensuring full patient comfort and minimizing pain. In some cases, when the patient experiences significant anxiety, sedation may be used to provide additional relaxation.
Extraction Procedure
- Gum Incision: The oral surgeon makes a small incision in the gum to access the tooth.
- Tooth Removal: Depending on the position and condition of the tooth, it may need to be sectioned into smaller pieces to facilitate removal. The procedure is carried out with the utmost precision to minimize damage to surrounding tissues.
- Wound Closure: After the tooth is removed, the wound is thoroughly cleaned and closed with sutures to accelerate healing and reduce the risk of infection.
After the Procedure
After the surgery, the patient receives detailed postoperative instructions, which include:
- Applying cold compresses to the outside of the cheek to reduce swelling.
- Avoiding hot, hard, and spicy foods for several days.
- Taking prescribed painkillers and anti-inflammatory medications.
- Regularly rinsing the mouth with a mild saline solution or a special mouth rinse to prevent infections.
- Limiting strenuous physical activity during the first few days after the procedure.
Follow-Up and Postoperative Care
A few days after the procedure, the patient should return for a follow-up visit, during which the dentist will assess the healing process, remove the stitches (if placed), and provide further instructions regarding oral hygiene and care of the extraction site.
Summary
Wisdom tooth extraction is often a necessary procedure to prevent serious health problems and ensure the patient’s comfort and oral health. Thanks to modern technologies and the experience of our specialists, these procedures are performed safely and effectively, with minimal discomfort for the patient.

Pre-prosthetic surgery is a specialized field of dentistry aimed at preparing the oral cavity for the placement of aesthetic, functional, and comfortable prosthetic restorations. This process is extremely important, as it ensures a stable and healthy foundation for dentures, bridges, crowns, and implants. Pre-prosthetic preparation involves several key stages and procedures that allow us to achieve optimal treatment outcomes.
Stages of Pre-Prosthetic Preparation
- Consultation and Diagnostics
The first step in preparing for prosthetic treatment is a thorough dental consultation. During this visit, we take a detailed medical history to understand the patient’s health background, expectations, and needs. We then perform a series of diagnostic tests, including X-rays (Panoramic, RVG) and CT scans, to accurately assess the condition of the oral cavity, bone, and soft tissues.
- Removal of Damaged Teeth
If the patient has damaged or unhealthy teeth that may interfere with prosthetic treatment, their removal is necessary. Tooth extractions are performed under computerized local anesthesia, ensuring comfort and minimizing pain. Thanks to modern surgical techniques, extractions are carried out quickly and safely.
- Bone Reshaping
After tooth removal, the next step is correcting any bone irregularities. Uneven bone structures can interfere with the proper placement of dentures or implants, so it is essential to provide a smooth and stable foundation. This process may include:
- Alveoloplasty: Surgical smoothing of the alveolar ridge by removing irregularities and sharp edges of the bone.
- Bone Augmentation: In cases of significant bone loss, we use bone regeneration techniques, such as grafting, to rebuild bone structure and volume.
- Removal of Pathological Changes
Pathological changes in the bone and soft tissues, such as cysts, tumors, or enlarged gums, must be removed before prosthetic treatment begins. The oral surgeon thoroughly cleans and removes these lesions, ensuring a healthy foundation for future prosthetic restorations.
- Soft Tissue Correction
Pre-prosthetic preparation also involves the correction of oral soft tissues. This may include:
- Gingivoplasty: Gum reshaping to achieve the correct contour and aesthetics.
- Frenectomy: Correction of lip and tongue frenula, which may affect the stability and comfort of dentures.
- Evaluation and Prosthetic Treatment Planning
After completing the surgical procedures, we perform a final assessment of the patient’s oral condition. Based on this, we develop a detailed prosthetic treatment plan tailored to the patient’s individual needs and expectations. This plan may include:
- Fabrication of fixed or removable dentures
- Placement of crowns and bridges
- Dental implantation

Advantages of Pre-Prosthetic Surgery
Pre-prosthetic surgery offers numerous benefits, including:
- Better Stability and Comfort of Dentures: A smooth and properly prepared bone foundation ensures improved stability and comfort when wearing dentures.
- Improved Aesthetics: Soft tissue correction and removal of pathological changes enhance the appearance of the oral cavity and smile.
- Reduced Risk of Complications: Removing damaged teeth and pathological changes lowers the risk of complications such as infections or inflammation.
Summary
Preparation for prosthetic treatment is a key stage that determines the success of the entire prosthetic process. In our clinic, we approach each patient individually, ensuring that every stage of preparation is carried out with the utmost care and precision. Thanks to advanced surgical techniques and the experience of our specialists, we provide patients with optimal conditions for prosthetic treatment, which translate into comfort, aesthetics, and functionality of prosthetic restorations.
Gingivoplasty is a surgical procedure that involves reshaping and contouring the gums to improve the aesthetics of the smile. The treatment is bloodless, safe, and painless, with immediate and long-lasting results.
Procedure Steps
- Consultation and Diagnostics
- Before the procedure, we conduct a detailed consultation with the patient to assess the condition of the gums and teeth, as well as to discuss the desired outcome of the smile.
- We take X-rays and perform other diagnostic tests to precisely evaluate the anatomy of the gums and teeth.
- Anesthesia
- The procedure is performed under local anesthesia, ensuring the patient’s full comfort and eliminating pain.
- Gum Reshaping
- The surgeon precisely removes excess gum tissue using specialized instruments or a laser, reshaping the gum line to visually expose more of the tooth.
- The entire process is carefully controlled and monitored to achieve a symmetrical and natural gum appearance.
- Wound Closure
- When a laser is used, stitches are usually not required, as the laser coagulates the tissue, minimizing bleeding and accelerating healing.


Benefits of Gingivoplasty
- Improved Smile Aesthetics: Correcting the gum line significantly enhances the smile, making it more harmonious and attractive.
- Quick Recovery Time: The procedure is minimally invasive, which means a fast recovery and minimal discomfort afterward.
- Safety: The treatment is safe and precise, minimizing the risk of complications.
- Long-Lasting Results: The effects of the procedure are long-lasting, allowing patients to enjoy a beautiful smile for many years.
Post-Treatment Care
After the procedure, the patient receives detailed oral care instructions to ensure smooth and quick healing:
- Avoiding hard and spicy foods: For a few days after the procedure, patients should avoid foods that may irritate the gums.
- Gentle oral hygiene: Patients should brush their teeth gently and avoid vigorous brushing of the treated area.
- Regular mouth rinsing: The use of special mouth rinses is recommended to support healing and prevent infections.
Follow-Up Consultations
Regular follow-up consultations allow us to monitor the healing process and evaluate the results of the procedure. If necessary, we perform additional adjustments to ensure complete patient satisfaction.
Summary
Gingivoplasty is an effective way to improve the aesthetics of your smile and boost self-confidence. At our clinic, we make sure that every procedure is performed with the highest precision and attention to patient comfort. Thanks to modern technology and the experience of our specialists, we can provide patients with a beautiful and healthy smile.

What are frenula?
Frenula are folds of the mucous membrane connecting the inner surface of the lips to the bones of the maxilla or mandible (in the case of labial frenula) and the underside of the tongue to the floor of the mouth (in the case of the lingual frenulum). They play an important role in regulating the mobility of the lips and tongue, which is why their shape, thickness, and attachment site are crucial for the proper functioning of the masticatory system.
Abnormalities and their impact on health
Abnormalities in the structure of frenula may take various forms:
- Thickening and abnormal shape – the folds may have a triangular or fan-like shape.
- Incorrect attachment – the frenulum may attach too close to the tooth necks or to the ridge of the alveolar process.
- Shortened lingual frenulum – limits tongue mobility, which may cause speech problems and the development of malocclusion.
- Overgrown upper labial frenulum – may result in a diastema (gap between the incisors) and also increase the risk of inflammation, gum recession, and tooth decay.
The frenuloplasty procedure
Frenuloplasty is a quick, painless procedure to correct frenula that takes only 2–3 minutes. It is performed without bleeding and does not require sutures. The procedure can be carried out in patients as young as 5 years old, improving both the aesthetics and functionality of the masticatory system.

Apicoectomy (root-end resection) is an effective method of treating inflammatory conditions in the periapical tissues, which may occur after improperly performed root canal treatment. This advanced surgical procedure helps save a tooth from extraction by eliminating the source of infection and restoring oral health.
Causes and Symptoms of Inflammatory Conditions
Inflammatory conditions in the periapical tissues can be caused by various factors, such as:
- Improperly performed root canal treatment
- Cracks or fractures of the tooth root
- Chronic bacterial infections
- Periapical cysts and granulomas
Symptoms of these inflammatory conditions include pain, swelling, gum redness, as well as abscesses and fistulas in the oral cavity. If left untreated, the inflammation can lead to tooth loss and the spread of infection to other parts of the body.


Course of the Apicoectomy Procedure
- Diagnostics and Planning
- Before performing the procedure, we carry out detailed diagnostic tests, including X-rays and cone-beam computed tomography (CBCT), to thoroughly assess the condition of the tooth root and surrounding tissues.
- Anesthesia
- The procedure is performed under local anesthesia, ensuring the patient’s full comfort and minimizing pain.
- Gum Incision and Mucosal Flap Reflection
- The surgeon makes an incision in the gum near the tooth and reflects the mucosal flap to gain access to the root apex.
- Removal of Infected Tissue and Root-End Resection
- The surgeon removes the infected periapical tissue and resects the root tip. This procedure eliminates the source of infection and prevents recurrence.
- Filling the Defect with Bone Substitute Material
- The defect left after the resection is filled with a bone substitute material, which supports bone regeneration and accelerates the healing process.
- Wound Closure
- Finally, the wound is carefully cleaned and closed with sutures to ensure quick and uncomplicated healing.
Post-Operative Care
After the procedure, the patient receives detailed post-operative instructions, including:
- Applying cold compresses to the outside of the cheek to reduce swelling
- Taking prescribed painkillers and anti-inflammatory medications
- Avoiding hard and spicy foods for a few days
- Gentle oral hygiene, including rinsing with a special mouthwash
Regular follow-up visits allow us to monitor the healing process and evaluate the results of the procedure.
Bone Regeneration
Bone regeneration is a key element in preparing the oral cavity for further implantology and prosthetic procedures. In our clinic, we use advanced bone regeneration techniques that allow the reconstruction of lost bone tissue and provide a stable foundation for implants.
Bone Regeneration Techniques
- Biomaterials
- We use various biomaterials, such as synthetic bone, xenografts (animal-derived materials), and allografts (human-derived materials). These biomaterials support the natural bone regeneration process by creating a structure on which new bone tissue can develop.
- Growth Factors from the Patient’s Blood
- An innovative method using growth factors obtained from the patient’s blood (PRF – Platelet-Rich Fibrin) significantly accelerates the tissue regeneration process. Growth factors stimulate cells to multiply and form new bone tissue, which increases the effectiveness of the procedure.
- Bone Grafts
- In some cases, a bone graft is necessary to rebuild missing bone. Grafts may be autogenous (taken from the patient), allogeneic (from a donor), or xenogeneic (from an animal source).

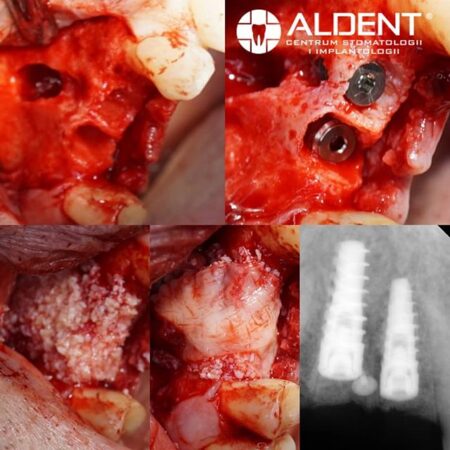
Bone Regeneration Procedure
- Consultation and Planning
- We conduct a detailed consultation to assess the condition of the bone and develop an individualized treatment plan.
- Preparation for the Procedure
- Before the procedure, we perform the necessary diagnostic tests to precisely evaluate the area that requires regeneration.
- Anesthesia and Procedure
- The procedure is carried out under local anesthesia, ensuring full patient comfort. The oral surgeon applies biomaterials or performs a bone graft in the area that requires regeneration.
- Post-Operative Care
- After the procedure, the patient receives detailed post-operative care instructions as well as prescribed medications to support the healing process and bone regeneration.
Open and Closed Methods
Sinus lift is a procedure that allows for an increase in the volume of bone tissue in the maxillary sinuses, which is crucial for performing implant procedures in areas with insufficient bone.
Procedure Steps
- Consultation and Planning
- Before the procedure, we carry out a detailed consultation and diagnostic assessment to carefully evaluate the anatomy of the maxillary sinuses and plan the appropriate sinus lift method.
- Open Sinus Lift Method
- This method is used when a significant increase in bone volume is required. The surgeon makes a small incision in the gum to access the maxillary sinus, then gently lifts the sinus membrane and introduces a bone substitute material, which stimulates the formation of new bone tissue.
- Closed Sinus Lift Method
- This method is less invasive and is used when only a small amount of additional bone tissue is needed. The bone substitute material is introduced through the extraction site or a specially prepared opening in the bone.
- Anesthesia and Procedure
- Both sinus lift methods are performed under local anesthesia, ensuring patient comfort and minimizing pain.
- Post-Operative Care
- After the procedure, the patient receives detailed post-operative care instructions, including avoiding strenuous physical activity, taking prescribed painkillers and anti-inflammatory medications, and regular mouth rinsing.


Summary
Apicoectomy, bone regeneration, and sinus lift procedures are key elements of modern oral surgery. Thanks to advanced techniques and the experience of our specialists, we are able to provide patients with effective treatment that restores oral health and prepares them for further implant and prosthetic procedures.
Would you like to schedule an appointment?
FAQ
What are the indications for wisdom tooth removal?
The main indications for wisdom tooth (third molar) extraction include: pain, recurrent infections, difficulty maintaining proper oral hygiene, untreatable tooth decay, and pressure on neighboring teeth that can cause shifting or damage. Wisdom teeth are also often removed as part of orthodontic treatment. At CSK ALDENT in Lublin, our oral surgeons carefully evaluate each case individually to ensure the best dental care.
When is the best time to remove wisdom teeth?
When do we perform bone augmentation?
Does tooth extraction hurt?
Why is surgical treatment at CSK ALDENT painless?
Should I remove wisdom teeth if they don’t hurt?
What is a dental implant?
How long does tooth extraction take?

Implantology
Oral surgery
Implant prosthetics

Specialist in oral surgery
Implantology

Conservative Dentistry
Microscopic Endodontics
Oral Surgery



